Scientists have likened a tumor to a wound that does not heal. Some of the same tissue responses that heal wounds operate in cancer to nurture a tumor’s growth. By understanding more about how tumors coopt the wound healing process, scientists are learning how to stop their growth and eliminate tumor cells through the natural and coordinated process of wound resolution. Likewise, inflammatory conditions have long been linked with certain cancers. We are now making progress in defining how inflammation alters tissues to support cancer initiation, and helps tumor cells adapt during metastasis or therapy resistance. A better mechanistic understanding will pave the way for prevention and treatment strategies that target inflammatory signals.
Scott Lowe and Dana Pe’er have teased apart the way gene-environment interactions create the precise conditions to support cancer development. By pairing new experimental models with single-cell sequencing, they were able to capture the spectrum of inflammation-related changes in pancreatic tissues. They showed that in the context of inflammation, normal pancreas cells with mutations in the KRAS gene undergo molecular changes, and that new cell-cell interactions between these transformed cells and the inflamed tissue environment promote tumor initiation.
Read more in the MSK News article or in the Science paper
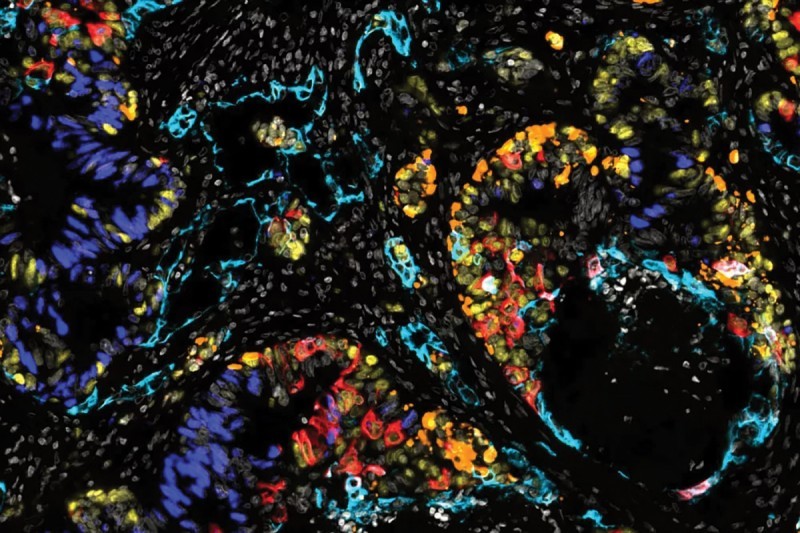
Resident stromal cells called fibroblasts support organ structure and function by producing extracellular matrix and signaling cues to mediate wound healing and maintain homeostasis. Mara Sherman characterizes the diversity of fibroblasts in the pancreas, and how these cells adopt distinct behaviors and microenvironmental interactions to promote pancreatic cancer progression. In one recent study, her lab used sophisticated genetically engineered mouse models and multiplex imaging techniques, to show that expression of the molecule KITL in fibroblasts maintains tissue architecture, acting as a microenvironmental tumor suppressor. Without KITL, the stromal cells gain inflammatory and pro-tumor features, accompanying tumor growth.
Read more in the MSK News article or in the Cancer Discovery paper
Lineage plasticity is a clinically challenging phenomenon in which cancer cells undergo a dramatic change in identity. Charles Sawyers studies lineage plasticity as a means of resistance to anti-androgen therapy in prostate cancer, by transitioning from a luminal identity into other cell states that are not dependent on androgen signaling. They uncovered an intriguing link between gain of plasticity and expression of inflammatory pathways, and in preclinical experiments showed that drugs targeting inflammatory signaling could block lineage plasticity, as a potential treatment strategy for resistant disease.
Read more in the MSK News article or in the Science paper
Joan Massagué and collaborators have shown that injury repair and regenerative programs are co-opted during metastatic progression in multiple cancer types. Together with Karuna Ganesh, they found that metastasis-initiating cells in colorectal cancer expressed the cell surface molecule L1CAM, which allows the cells to more easily detach from their resident tissue and migrate to other organs. Since L1CAM is not present in healthy tissue, it holds promise as a biomarker to detect metastasis and a target for anti-metastasis drugs.
Read more in the MSK News article or in the Nature Cancer paper
The spectacular success of immunotherapy has shown the power of the immune system to fight cancer. But the immune system doesn’t operate as singular force; it’s more like a complex network of cell types and molecules, that can perform many different functions within tumor tissues and throughout the whole body. Empowered by advanced single-cell and spatial biology tools, scientists will focus on mapping these circuits, to better understand how to improve immunotherapy.
Immune checkpoint inhibitors work to release a molecular brake on T cells, so they can recognize and eliminate cancers. Yet immunotherapy is not always effective, even when T cells are present in tumor tissues. Immunologist Andrea Scheitinger found that specialized physical interactions between T cells and dendritic cells to form “immune triads” were needed for effective immunotherapy response. This work suggests that next-generation treatments could be designed to spatially reorganize immune cells in the tumor microenvironment, to therapeutically induce triad formation and boost anti-tumor immunity.
Read more in the MSK News article or in the Cancer Cell paper
Frederic Geissmann and colleagues including Joan Massagué, Joseph Sun, Robert Benezra, and Christine Iacobuzio-Donahue characterized the role of the ID3 protein in dictating the way specialized Kupffer cells that reside in the liver mount a response against tumor cells. The Kupffer cells recruit and interact with other immune cells, to form an immune niche that limits tumor growth in the liver, a common site of metastasis for multiple cancer types.
Read more in the Nature paper
Alexander Rudensky studies regulatory T cells, which have well-known influence on the behavior of other T cell populations in autoimmunity and cancer. Along with collaborators including Dana Pe’er, Charles Rudin and Gabrielle Rizzuto, they found that regulatory T cells also functionally interact in important ways with stromal and vascular cells in the tumor microenvironment, and showed that a drug combination that altered this network of ‘accessory’ cells in the tumor tissue was effective as a lung cancer therapy in preclinical studies.
Read more in the Nature Immunology paper
Understanding why some cancer types, and individual patients, respond to immunotherapy while others do not is a paramount clinical challenge. Sohrab Shah, with Dmitriy Zamarin and interdisciplinary collaborators across MSK, performed multi-modal profiling in human high-grade serous ovarian cancers across several anatomic sites, to gain insights into this question. With this highly detailed annotation of the tissues, they were able to pinpoint both tumor genomic features and localized immune cell interactions that contributed to escape from anti-tumor immunity.
Read more in the MSK News article or in the Nature paper
Andy Minn is the inaugural Chair of the Immuno-Oncology Program at MSK, and has made key contributions to our understanding of immunotherapy response and resistance. His work has revealed context-dependent effects of interferon signaling in cancer cells and immune cells, underscoring the complex tissue dynamics at play when studying cancer biology and treatment. He has also explored how certain therapies including radiation can stimulate “viral mimicry,” which leads T cells to recognize and attack cancer cells in a manner similar to a viral infection response. His ongoing translational research aims to guide new and combinatorial strategies to rewire tumor-immune crosstalk for more effective immunotherapy.
Altered cellular metabolism enables cancer cells to adapt to conditions of rapid tumor growth. At the same time, stromal and immune cells coexisting with developing tumors may respond or contribute to changes in local nutrient resources in ways that can either promote or suppress tumor growth. Using new methods to understand these complex dynamics will help to understand how metabolism affects overall tissue behavior and how this can be exploited to develop clinical diagnostic tools and new cancer treatments.
Over the course of mounting an immune response to a developing cancer, T cells can become ‘exhausted,’ and lose their tumor-fighting capabilities. Santosh Vardhana and Craig Thompson identified key metabolic changes that occur in T cells that are chronically stimulated – as is often the case in the local tumor microenvironment – linked to this impaired function. An antioxidant treatment that re-balanced T cell metabolism led to improved anti-tumor immune response.
Read more in the MSK News article or in the Nature Immunology paper
Lydia Finley studies cellular metabolism in normal development and cancer, and has shown that skin stem cells with cancer-predisposing mutations have distinct needs for an extracellular source of serine, a key metabolic building block, that drives squamous cell carcinoma development. When extracellular serine was depleted and premalignant cells were required to produce their own serine, this triggered other biochemical changes that promoted cell differentiation and suppressed tumor initiation, demonstrating that beyond just fueling cellular growth, metabolic adaptations can support tumor progression by redirecting epigenetics and cell fate regulation toward malignancy.
Read more in the MSK News article or in the Nature Cell Biology paper
Joseph Sun studies natural killer cells, and how they contribute to anti-tumor immunity. His lab performed a study in mice showing that a period of fasting induced changes in the metabolic function of natural killer cells as well as their trafficking throughout the body, which led to new encounters with other immune cells that strengthened NK anti-tumor immune responses. These preclinical results support further exploration of dietary or pharmacologic strategies that alter metabolism to enhance immunotherapy.
Read more in the MSK News article or in the Immunity paper
The cellular composition in tumors and in normal tissues is not uniform, and variations in the cellular landscape could also be correlated with spatial heterogeneity of metabolic features. Ed Reznik, Ari Hakimi and colleagues analyzed multi-region tissue samples from patients with clear cell renal cell carcinoma, finding that metabolite fluctuations were influenced by the particular composition of local immune cells, and that certain metabolites could be linked to therapy response in clinical datasets.
Read more in the Cell Metabolism paper
Metastatic cells often coopt developmental pathways that are usually active only during embryonic development. Cancer cells can tap into these pathways through epigenetic means. Scientists at MSK are using powerful single-cell technologies to capture the spectrum of cell states that emerge across key time points in normal development and in cancer progression. Combining observations from cancer and developmental biology will map these changes, with the aim of blocking cancer cells’ abilities to rely on these pathways for their growth and metastasis.
Developmental biologist Kat Hadjantonakis and computational biologist Dana Pe’er have conducted high-resolution mapping of embryonic development in mouse models, defining regulators of lineage plasticity and differentiation. As organs form and adopt specialized functions, lineage plasticity is decreased, while differentiation pathways are turned on. These single-cell maps provide valuable insights about the earliest stages of normal development, and potential reference points for mechanisms that become re-activated in cancer progression, including plasticity.
Read more in the MSK News article or in the Nature paper
Karuna Ganesh studies metastasis in colorectal cancer, and along with Dana Pe’er and several clinical colleagues, performed single-cell profiling of patient-matched tumor samples in an effort to understand differences in the biology between primary and metastatic tumors, that make the latter more aggressive and resistant to treatment. They found that a cell state with features similar to fetal progenitors was prominent in metastases, and that emergence of this cell state enabled further lineage plasticity and progressive disease.
Read more in the MSK News article or in the Nature paper
Luis Parada performed detailed single-cell profiling of neural stem cells in the brain subventricular zone across the adult life span in mice, finding that functional properties of these cells varied based on the anatomic subregion of the SVZ and increased age. These neural stem cells are linked to brain injury repair and implicated in the formation of gliomas; thus, this work is a valuable resource to better understand their biology, and to identify determinants of susceptibility or transition to disease.
Read more in the PNAS paper
With advances in experimental models and systems biology approaches, we can begin to take on cancer ecosystems at the whole-body and macroenvironment level. There is growing appreciation for understanding how the nervous system and gut microbiome influence cancer biology, and reciprocally how cancer itself or cancer treatments affect other organ systems. Major questions remain about how aging and lifestyle factors such as obesity, stress, or environmental exposures manifest at the cellular and molecular level, and how we can translate these insights into improved outcomes through risk reducing or therapeutic interventions.
Aging is a well-known risk factor for developing cancer, but the complex effects of aging on normal tissue physiology and disease are not well understood. Tuomas Tammela recently uncovered that old age can have a surprising protective role against lung cancer in mouse models, which was related to a change in iron metabolism that reduced fitness in the tissue stem cells of old mice. As these stem cells are the source of lung cancer, their impaired regenerative ability led to reduced cancer incidence compared to younger mice.
Read more in the MSK News article or in the Nature paper
The interaction between cancer and the nervous system is an exciting and rapidly advancing field of study, enabled by advanced imaging technologies and the application of experimental neuroscience tools. Kathryn Taylor, an Assistant Member in the Cancer Biology & Genetics program at Sloan Kettering Institute, is focusing her new lab on uncovering cancer-neuron interactions in pediatric and young adult cancers, building on her findings that childhood gliomas coopt neuronal signaling to fuel malignant growth. Inhibition of such malignant rewiring could open up translational opportunities in cancer neuroscience.[Image: Taylor headshot]
Ross Levine studies clonal hematopoiesis, a common condition in older individuals that involves the accumulation of blood cells with certain mutations over time and is linked to increased risk of blood cancer as well as heart disease. Dr. Levine’s research team recently developed a novel experimental model system for clonal hematopoiesis, in order to better understand the biology of mutant cells and the factors that lead to malignant progression, and to identify potential targets for early intervention or management of clonal hematopoiesis.
Read more in the Cancer Discovery paper
While conventional cancer treatments are aimed at tumor cells directly, the paradigm of immunotherapy demonstrated the great potential in treatments that harness the tumor microenvironment to destroy cancer cells. Powerful and unexpected new drug targets can be revealed as we explore cancer ecosystems biology in greater detail. Researchers are adopting CRISPR-based approaches to screen the universe of all possible ligand/receptor communications in advanced in vivo or organoid models that can retain features of the complex cancer ecosystem. Moreover, systems-level profiling in clinical samples has the potential to uncover actionable insights into how the ecosystem contributes to treatment failure, or the emergence of resistance.
Adrienne Boire led a study identifying a unique property of the cerebral spinal fluid ecosystem that could be exploited as an anti-metastasis therapy. Along with colleagues Dana Pe’er and Christine Iacobuzio-Donahue, Dr. Boire combined analyses of CSF metastases from patient samples and mouse models to identify the protein LCN-2 expressed by cancer cells that enables them to survive in the CSF by competing for iron resources with resident macrophages. This work led to the development of LCN-2 inhibitors that effectively block this survival advantage, which is now being tested in patients.
Read more in the MSK News article or in the Science paper
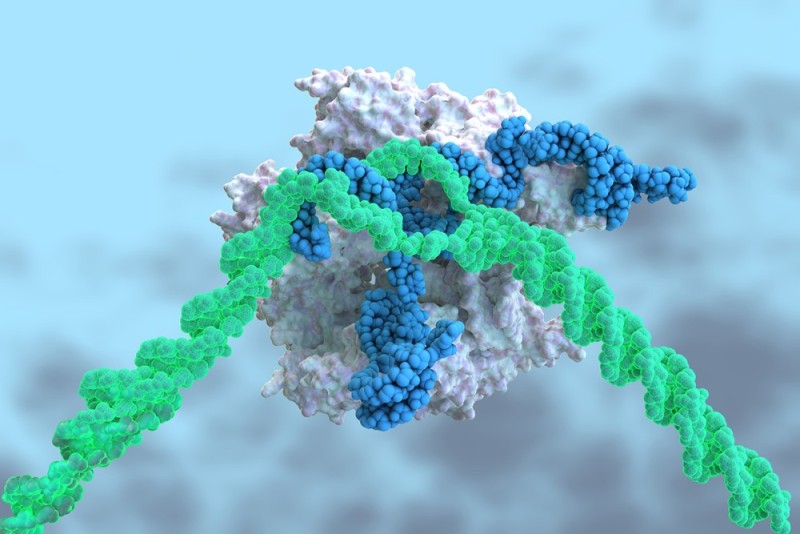
Joan Massagué and colleagues including Joseph Sun, Scott Lowe, Dana Pe’er, and Christine Iacobuzio-Donahue pursued a strategy to target and eliminate dormant metastatic cells, by performing an in vivo CRISPR-Cas9 screen specifically designed to identify molecules involved in crosstalk between dormant cells and nearby immune cells. In preclinical experiments, they show that treatment with a STING agonist made dormant cells more visible to the immune system and suppressed metastasis.
Read more in the MSK News article or in the Nature paper
Thomas Norman is a computational biologist who has pioneered functional genomics platforms such as Perturb-seq and Multiome Perturb-seq that enable large scale identification of potentially targetable vulnerabilities in cancer. Collaborative efforts are underway to adapt and enhance these tools for at-scale characterization of novel therapeutic targets, by conducting functional screening in cancer ecosystems models, including organoids and mouse tumor models.
Read more in the recent Cell Systems paper
Daniel Heller and David Scheinberg teamed up to improve the specificity of CAR-T cell therapy for solid tumors, using special properties of the tumor microenvironment. Since the molecule P-selectin is present on blood vessels in tumors but not in healthy tissue, they designed “microenvironment actuated” CAR-T cells to recognize a tumor cell target as well as P-selectin, that showed enhanced tumor homing and reduced off-target toxicities.
Read more in MSK News or in the Science Advances paper