One of the ways scientists are trying to improve cancer treatments is by better equipping the body’s own immune system to fight off the disease – and a new study identifies a molecular switch that can do just that.
Through an extensive screening process in which genes in cancer cells in the lab were ‘switched off’ to pinpoint their effects, researchers found that a gene producing the TAK1 protein was crucial for cancer cells to evade immune attack.
Further tests on cancer cells in mice with normal immune systems then confirmed how vital TAK1 is for cancer: Tumors in mice without this protein grew more slowly, and the mice survived for longer, on average.
Related: Powerful Anti-Cancer Drug Discovered Inside Japanese Tree Frog
The research team from institutions in Australia and Ireland believes their findings could aid in the development of future treatments. Medications could potentially directly target TAK1 production, and ‘flip’ this molecular switch.
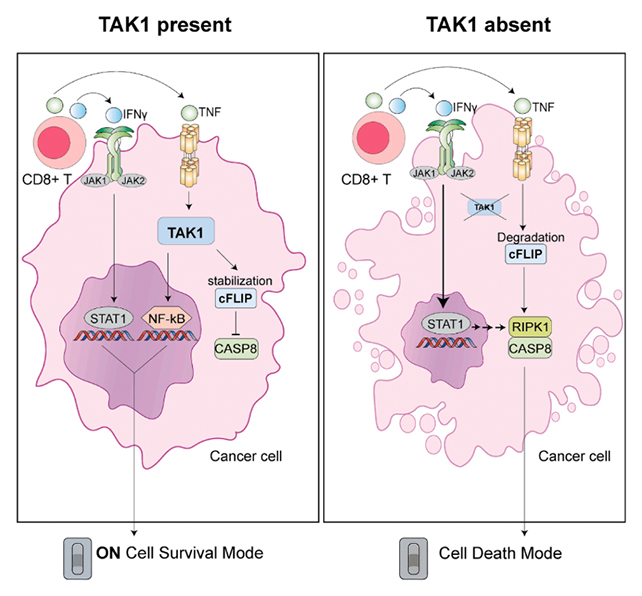
“It is known that TAK1 promotes cancer cell survival and blocks cell death,” says cancer cell biologist Anne Huber, from the Olivia Newton-John Cancer Research Institute (ONJCRI) in Australia.
“However, we didn’t know that cancer cells use this tactic to avoid killing by the immune system.”
Huber and colleagues examined in greater detail the mechanisms underlying TAK1’s effect. Specifically, it protects cancer cells from the activity of CD8⁺ T cells, immune cells that clear out damaged cells and kill deadly invaders like cancer cells.
One way these CD8⁺ T cells are effective is by releasing chemical signals called cytokines, which can more readily reach their targets when TAK1 is absent.
Knowing how this process works in detail could help scientists better harness it for cancer treatments. When TAK1 is removed, cancer cells are essentially trying to survive without one of their best bodyguards.
It’s worth emphasizing that this study involved cancer cells developed in the lab and tumors in mouse models. There’s reason to believe the results can translate to humans, but that work still needs to be carried out and extended to a broader range of cancers (this study looked mainly at melanoma).
However, these findings are encouraging. One of the benefits of immunotherapy approaches to tackle tumors is that they lean more heavily on the body’s own defences, rather than chemotherapy drugs or radiation.
Patient safety is always a crucial consideration whenever it comes to cancer-fighting treatments.
Stopping the production of TAK1 may be feasible in the future, but investigators will need to determine potential adverse health effects on the rest of the body and weigh them against the benefits.
“Blocking TAK1 could make current immunotherapies more effective by stripping tumors of this protection,” says medical biologist Tirta Djajawi, from ONJCRI.
“TAK1 is like a shock absorber that lets cancer cells survive the immune system’s hardest hits. Remove it, and the tumor collapses under the force of immune attack.”
The research has been published in Cell Reports.
